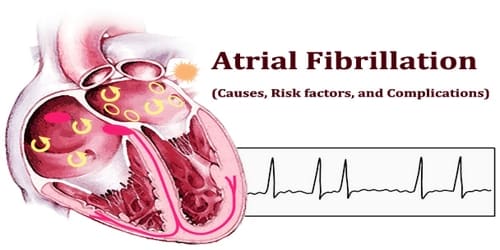
Atrial fibrillation (Causes, Risk factors, and Complications)
Definition: Atrial fibrillation (also called AFib or AF) is an abnormal heart rhythm characterized by the rapid and irregular beating of the atria. Instead of the SA node (sinus node) directing the electrical rhythm, many different impulses rapidly fire at once, causing a very fast, chaotic rhythm in the atria. Because the electrical impulses are so fast and chaotic, the atria cannot contract and/or squeeze blood effectively into the ventricle.
Often it starts as brief periods of abnormal beating which become longer and possibly constant over time. Often episodes have no symptoms. Occasionally there may be heart palpitations, fainting, lightheadedness, shortness of breath, or chest pain. The disease is associated with an increased risk of heart failure, dementia, and stroke. It is a type of supraventricular tachycardia.
Atrial fibrillation is a type of arrhythmia. There are four main types of atrial fibrillation—paroxysmal, persistent, and long-term persistent and permanent atrial fibrillation. The type of atrial fibrillation that people have depends on how often atrial fibrillation occurs and how it responds to treatment.
Episodes of atrial fibrillation can come and go, or you may develop atrial fibrillation that doesn’t go away and may require treatment. Although atrial fibrillation itself usually isn’t life-threatening, it is a serious medical condition that sometimes requires emergency treatment.
It may lead to complications. Atrial fibrillation can lead to blood clots forming in the heart that may circulate to other organs and lead to blocked blood flow (ischemia).
Atrial fibrillation is the most common serious abnormal heart rhythm. In the developing world, about 0.6% of males and 0.4% of females are affected. The percentage of people with AF increases with age with 0.1% under 50 years old, 4% between 60 and 70 years old, and 14% over 80 years old being affected.
Treatments for atrial fibrillation may include medications and other interventions to try to alter the heart’s electrical system.
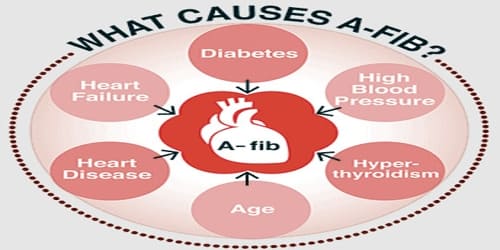
Causes and Risk factors of Atrial fibrillation: Atrial fibrillation (AF) is linked to several forms of cardiovascular disease, but may occur in otherwise normal hearts. Changes to the heart’s tissue and to its electrical signals most often cause atrial fibrillation. To understand atrial fibrillation, it helps to know how the heart works. When the heart’s tissue or signaling is damaged, the regular pumping of the heart muscle becomes fast and irregular. Most often, damage to the heart is the result of other conditions such as high blood pressure and ischemic heart disease.
Abnormalities or damage to the heart’s structure is the most common cause of atrial fibrillation. Possible causes of atrial fibrillation include:
- High blood pressure
- Heart attacks
- Coronary artery disease
- Abnormal heart valves
- Heart defects you’re born with (congenital)
- An overactive thyroid gland or other metabolic imbalance
- Exposure to stimulants, such as medications, caffeine, tobacco or alcohol
- Sick sinus syndrome — improper functioning of the heart’s natural pacemaker
- Lung diseases
- Previous heart surgery
- Viral infections
- Stress due to pneumonia, surgery or other illnesses
- Sleep apnea
In at least 10 percent of the cases, no underlying heart disease is found. In these cases, AF may be related to alcohol or excessive caffeine use, stress, certain drugs, electrolyte or metabolic imbalances, severe infections, or genetic factors. In some cases, no cause can be found.
The risk of AF increases with age, particularly after age 60.
Certain factors may increase our risk of developing atrial fibrillation. High blood pressure and valvular heart disease are the most common alterable risk factors for AF. Age, family history and genetics, lifestyle, heart disease or other medical conditions, race, sex, and a history of surgery can all raise our risk of developing the structural and electrical anomalies that cause atrial fibrillation. Even in a healthy heart, a fast or slow heart rate—from exercising or sleeping, for example—can trigger atrial fibrillation.
People may be at risk for atrial fibrillation in the early days and weeks after surgery of the heart, lungs, or esophagus. Surgery to correct a congenital heart defect can also raise the risk of atrial fibrillation. This can happen years after a childhood surgery or when they have surgery as an adult to correct a lifelong condition.
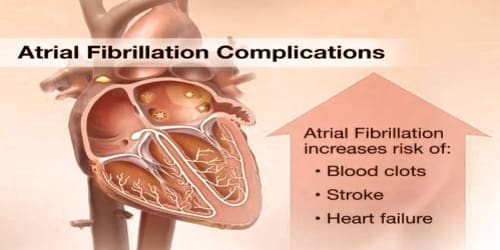
Complications of Atrial fibrillation: Some people live for years with atrial fibrillation without problems. AF can decrease the heart’s pumping ability. The irregularity can make the heart work less efficiently. In addition, atrial fibrillation that occurs over a long period of time can significantly weaken the heart and lead to heart failure. Sometimes atrial fibrillation can lead to the following complications:
- Stroke. In atrial fibrillation, the chaotic rhythm may cause blood to pool in people’s heart’s upper chambers (atria) and form clots. If a blood clot forms, it could dislodge from their heart and travel to their brain. There it might block blood flow, causing a stroke.
- Heart failure. Atrial fibrillation, especially if not controlled, may weaken the heart and lead to heart failure — a condition in which people’s heart can’t circulate enough blood to meet their body’s needs.
People with atrial fibrillation are 5 to 7 times more likely to have a stroke than the general population. Clots can also travel to other parts of the body (kidneys, heart, intestines), and cause other damage.
Information Source: