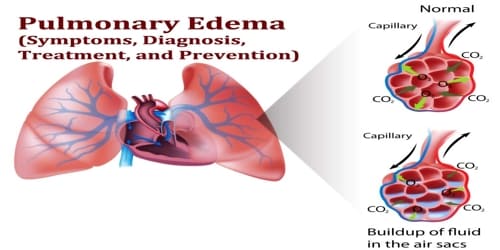
Pulmonary Edema (Symptoms, Diagnosis, Treatment, and Prevention)
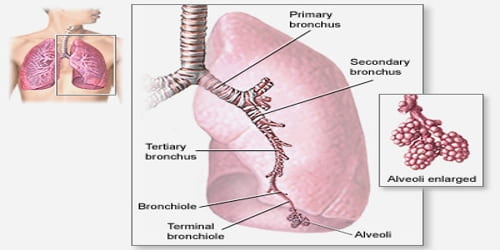
Definition: Pulmonary Edema, also known as lung congestion, occurs when fluid accumulates in the air sacs of the lungs – the alveoli – making it difficult to breathe. This interferes with gas exchange and can cause respiratory failure. It is a cardinal feature of congestive heart failure.
The term edema is from the Greek οἴδημα (oídēma, “swelling”), from οἰδέω (oidéō, “I swell”).
In most cases, heart problems cause pulmonary edema. But fluid can accumulate for other reasons, including pneumonia, exposure to certain toxins and medications, trauma to the chest wall, and visiting or exercising at high elevations.
Some external factors can also put extra pressure on the heart and lungs and cause pulmonary edema. These outside factors are:
- high altitude exposure
- illicit drug use or drug overdose
- lung damage caused by the inhalation of toxins
- severe trauma
- major injury
- near drowning
Treatment is focused on three aspects: firstly improving respiratory function, secondly, treating the underlying cause, and thirdly avoiding further damage to the lung. Pulmonary edema, especially acute, can lead to fatal respiratory distress or cardiac arrest due to hypoxia.
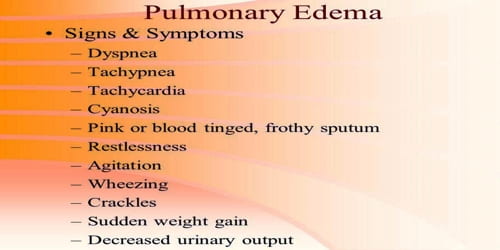
Signs and Symptoms of Pulmonary Edema: The most common symptom of pulmonary edema is difficulty breathing, but may include other symptoms such as coughing up blood (classically seen as pink, frothy sputum), excessive sweating, anxiety, and pale skin.
Other signs and symptoms of acute pulmonary edema can include:
- a cough, often with a pink frothy sputum
- excessive sweating
- anxiety and restlessness
- feelings of suffocation
- pale skin
- wheezing
- rapid or irregular heart rhythm (palpitations)
- chest pain
Typical symptoms include:
- difficulty breathing when lying flat (orthopnea)
- swelling (edema) of feet or legs
- rapid weight gain due to the accumulation of excess fluid
- paroxysmal nocturnal dyspnea – episodes of severe sudden breathlessness at night
- fatigue
- increased breathlessness with physical activity
If pulmonary edema continues, it can raise the pressure in the pulmonary artery (pulmonary hypertension), and eventually, the right ventricle in our heart becomes weak and begins to fail.

Diagnosis and Treatment of Pulmonary edema: There is no one single test for confirming that breathlessness is caused by pulmonary edema; indeed, in many cases, the cause of shortness of breath is probably multifactorial. The patient will undergo a physical exam first.
Examples of tests used in diagnosing pulmonary edema include:
- complete blood count
- echocardiogram, or an ultrasound, to check for abnormal heart activity
- chest X-ray to see fluid
- blood tests to check oxygen levels
- electrocardiogram (ECG) to look for heart rhythm problems or signs of a heart attack
Blood tests are performed for electrolytes (sodium, potassium) and markers of renal function (creatinine, urea). Liver enzymes, inflammatory markers (usually C-reactive protein) and a complete blood count as well as coagulation studies (PT, aPTT) are also typically requested. B-type natriuretic peptide (BNP) is available in many hospitals, sometimes even as a point-of-care test. Low levels of BNP (<100 pg/ml) suggest a cardiac cause is unlikely.
A CT scan of the chest may also be ordered.

Some cases of pulmonary edema may need treatment to assist in breathing. A machine will deliver oxygen under pressure to help get more air into the lungs. Sometimes this can be done with a mask or cannula, also called Continuous Positive Airway Pressure (CPAP).
Depending on the patient’s condition and the reason for their pulmonary edema, they may also receive one or more of the following medications:
- Morphine (MS Contin)
- Diuretics
- Blood pressure medications
Nitroglycerin is a preload reducer that helps decrease the pressure going into our heart. Medications such as nitroprusside (Nitropress) are afterload reducers that dilate our blood vessels and take a pressure load off our heart’s left ventricle.
Prevention of Pulmonary edema: Dexamethasone is in widespread use for the prevention of high altitude pulmonary edema. Sildenafil is used as a preventive treatment for altitude-induced pulmonary edema and pulmonary hypertension, the mechanism of action is via phosphodiesterase inhibition which raises cGMP, resulting in pulmonary arterial vasodilation and inhibition of smooth muscle cell proliferation.
The best way to try and prevent pulmonary edema is by taking good care of people’s health:
- Get a pneumonia vaccine.
- Get the flu vaccine, especially if they have heart problems or if they are an older adult.
- Remain on diuretics after an episode of pulmonary edema to prevent a reoccurrence.
People can also decrease their risk of heart failure, the most common cause of pulmonary edema:
- Visit their doctor regularly.
- Don’t smoke or use recreational drugs.
- Get regular exercise.
- Eat healthy foods.
- Maintain a normal weight.
Altitude-induced pulmonary edema can be minimized by making a gradual ascent, taking medications before traveling, and avoiding excess exertion while progressing to higher altitudes.
Information Source: