There are trillions of bacteria, viruses, and fungi in your body. They are referred to collectively as the microbiome. While some bacteria are associated with disease, others are vital to your immune system, heart, weight, and a variety of other health factors.
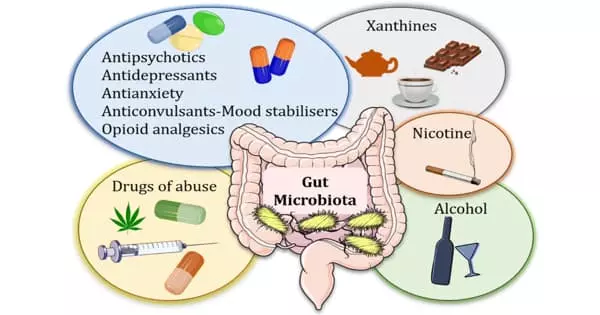
The human gut microbiome is a complex ecosystem that can mediate the human host’s interaction with their surroundings. The interaction between gut microbes and commonly used non-antibiotic drugs is complex and bidirectional: drugs can influence gut microbiome composition, but the gut microbiome can also influence an individual’s response to a drug by enzymatically transforming the drug’s structure and altering its bioavailability, bioactivity, or toxicity.
We are one of the most medicated generations of humans to have ever lived on Earth. Cardiometabolic diseases such as type 2 diabetes, obesity, and coronary artery disease continue to rise in prevalence and are now the leading cause of death worldwide. Affected people are frequently required to take multiple medications on a daily basis for months or even years.
The gut microbiome is made up of billions of microorganisms that are necessary for the body’s normal functioning. We studied the effects of 28 different drugs and several drug combinations. Many drugs have a negative impact on the composition and state of the gut bacteria, but others, such as aspirin, can have a positive impact on the gut microbiome.
Peer Bork
Many commonly used drugs have powerful effects on our gut microbes, according to researchers from the Bork group at EMBL Heidelberg, who collaborated with a European consortium involving more than twenty European institutes. Antibiotics and drugs used to treat cardiometabolic disorders are examples of these. The findings have been published in the journal Nature.
Many commonly used drugs have powerful effects on our gut microbes, according to researchers from the Bork group at EMBL Heidelberg, who collaborated with a European consortium involving more than twenty European institutes. Antibiotics and drugs used to treat cardiometabolic disorders are examples of these. The findings have been published in the journal Nature.
The gut microbiome is made up of billions of microorganisms that are necessary for the body’s normal functioning. “We studied the effects of 28 different drugs and several drug combinations,” Peer Bork, Director of Scientific Activities at EMBL Heidelberg, explained. “Many drugs have a negative impact on the composition and state of the gut bacteria, but others, such as aspirin, can have a positive impact on the gut microbiome. We discovered that drugs can have a greater impact on the host-microbiome than disease, diet, and smoking combined.”
While the negative and long-term effects of antibiotics on gut bacteria are well known, this study demonstrated that such effects are likely to accumulate over time. “We discovered that the gut microbiome of patients who received multiple courses of antibiotics over a five-year period became less healthy. This included signs of antimicrobial resistance “Sofia Forslund, a former postdoctoral fellow in the Bork group and now group leader at the Max Delbrück Center for Molecular Medicine (MDC) in Berlin, was a co-first author of the study.
“We wanted to separate the effect of diseases on host microbiomes from the effect of medications, especially in patients taking multiple drugs at the same time,” said co-first author and EMBL Heidelberg postdoctoral researcher Maria Zimmermann-Kogadeeva. “Being a part of the MetaCardis consortium allowed us to use multi-omics data from over 2000 patients with cardiometabolic diseases,” she continued. The large cohort also allowed the researchers to establish that drug dosage has a significant effect on the level of impact on the microbiome.
“We know that the microbiome can reflect a patient’s health status and provide a variety of biomarkers to assess disease severity. What is frequently overlooked, however, is that the medication used to treat disease also has an impact on the state of the microbiome “Rima Chakaroun, a clinician-scientist at the University of Leipzig Medical Center and one of the study’s lead authors, agreed. Dr. Chakaroun is a postdoctoral fellow at the University of Gothenburg’s Wallenberg Laboratory.
The researchers were able to separate the effects of drugs and disease by developing a statistical approach that accounts for the effects of multiple confounding factors. “We now have a robust methodological framework that allows us to eliminate many of the standard errors,” Professor Bork said. “This allowed us to demonstrate that medication can mask disease signatures and conceal potential biomarkers or therapeutic targets.”
The researchers hope that these findings will contribute to drug repurposing as well as the development of personalized treatment and prevention strategies.
The study drew on the expertise, knowledge, and approaches of experts from six different countries. “Working with an interdisciplinary team of clinicians, bioinformaticians, and computational systems biologists to advance our understanding of molecular interactions in cardiometabolic disease was very motivating,” said Dr. Zimmermann-Kogadeeva.