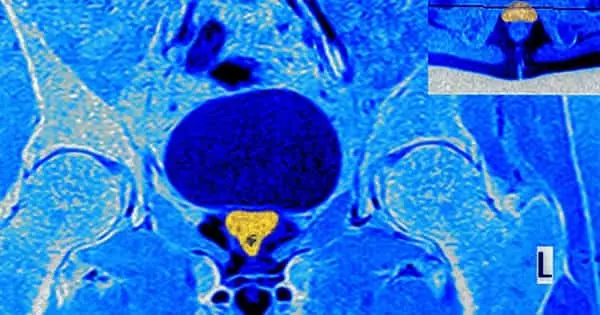
The majority of prostate cancers are discovered as a result of screening. Early prostate cancers rarely cause symptoms, but more advanced cancers are sometimes discovered as a result of the symptoms they cause. Maximum tumor diameter has been shown to correlate with a number of clinical outcome predictors in prostate cancer. Improving imaging processes will lead to more successful treatments and will aid in the reduction of morbidity in men with the disease.
According to a study published in the Journal of Urology, magnetic resonance imaging (MRI) is frequently used in the diagnosis and management of prostate cancer, but the method frequently underestimates tumor size. According to a UCLA Jonsson Comprehensive Cancer Center study, MRI is frequently used in the diagnosis and management of prostate cancer, but the method frequently underestimates tumor size.
A UCLA Jonsson Comprehensive Cancer Center-led study discovered that magnetic resonance imaging, or MRI, frequently underestimates the size of prostate tumors, potentially leading to undertreatment. The authors of the study discovered that such underestimation occurs most frequently when the MRI-measured tumor size is small and the PI-RADS score, which is used to classify lesions in prostate MRI analysis, is low.
A study has found that magnetic resonance imaging, or MRI, frequently underestimates the size of prostate tumors, potentially leading to undertreatment.
Both the MRI size measurement and the PI-RADS score must be accurate for prostate tumor treatments to be successful because they allow physicians to determine precisely where tumors end and the normal, healthy tissue surrounding them begins.
Prostate cancer is frequently diagnosed and managed using MRI. It is also being used to map and guide the delivery of new, highly targeted therapies that use freezing (cryotherapy), ultrasound (HIFU), and heat (laser ablation) to destroy cancerous tissue in the prostate gland while sparing healthy tissue.
In 441 men treated for prostate cancer, researchers compared MRI-measured tumor size to actual tumor size after prostate removal. The study included 441 men who had biopsy-proven prostate cancer and three or more index lesions on the Prostate Imaging Reporting and Data System version 2 (PI-RADSv2) and later underwent radical prostatectomy. They defined radiologic tumor size as the maximum tumor diameter determined by MRI and compared those measurements to those found in whole-mount histopathology following resection.
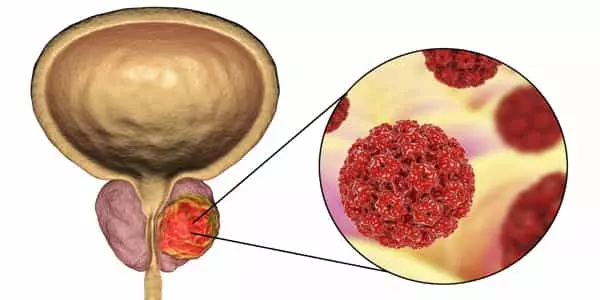
The 461 lesions identified from the 441 patients were included in the analysis. The average pathological tumor size was 2.37 cm, while the average radiologic tumor size was 1.57 cm. Despite the fact that tumor size was consistently underestimated in the radiologic setting, tumors that were smaller and had lower PI-RADSv2 scores tended to be underestimated more than others.
Pathologic prostate tumor size is frequently larger than indicated by 3 Tesla multiparametric magnetic resonance imaging (3T mpMRI), which has clinical implications for the use of such imaging for focal therapy.
Pathological tumor size was larger in cases where tumors were classified as grade 5 on the Gleason Grade Group (GG), with a mean change of 0.37 cm (P =.014) compared to GG grade 1 tumor. Lesions rated 5 on the PI-RADSv2 index had pathological tumor sizes that were 0.26 (P =.006) larger than PI-RADSv2 4 lesions. Tumors with a higher density of prostate-specific antigen were also larger.
Overall, there was little correlation in the cohort between radiologic tumor measurements and pathological tumor size. Correlation coefficients ranged from 0.1 to 0.65, according to the researchers. Inadequate tumor measurements can make it difficult for doctors to see where the tumor’s outer edges end and healthy tissue begins, potentially leading to insufficient treatment if the measurements are understated.
The authors concluded, “Multiparametric magnetic resonance imaging frequently underestimates pathological tumor size, and the degree of underestimation increases with smaller radiologic tumor size and lower PI-RADSv2 scores.”
As physicians estimate focal therapy treatment margins, they suggest that a larger ablation margin may be required for the treatment of smaller tumors and those rated low on the PI-RADSv2 scale. Improving the ability to predict ablation margins will allow for more successful treatments for men with prostate cancer and will help reduce morbidity associated with prostate cancer treatment.