About Malaria
Definition
Malaria is caused by Plasmodium parasites. The parasites are spread to people through the bites of infected female Anopheles mosquitoes, called “malaria vectors.” Malaria produces recurrent attacks of chills and fever. In severe cases it can cause yellow skin, seizures, coma, or death. Symptoms usually begin ten to fifteen days after being bitten. If not properly treated, people may have recurrences of the disease months later. In those who have recently survived an infection, reinfection usually causes milder symptoms. This partial resistance disappears over months to years if the person has no continuing exposure to malaria Malaria kills an estimated 660,000 people each year.
Malaria transmission occurs primarily between dusk and dawn because of the nocturnal feeding habits of Anopheles mosquitoes. One should therefore take protective measures to reduce contact with mosquitoes, especially during these hours. These measures include remaining in well-screened areas, using mosquito nets, and wearing clothes that cover most of the body.
Key Facts of Malaria –
- Malaria is a life-threatening disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes.
- In 2015, 91 countries and areas had ongoing malaria transmission.
- Malaria is preventable and curable, and increased efforts are dramatically reducing the malaria burden in many places.
- Between 2010 and 2015, malaria incidence among populations at risk (the rate of new cases) fell by 21% globally. In that same period, malaria mortality rates among populations at risk fell by 29% globally among all age groups and by 35% among children under 5.
- The WHO African Region carries a disproportionately high share of the global malaria burden. In 2015, the region was home to 90% of malaria cases and 92% of malaria deaths.
Signs, Symptoms and Causes of Malaria
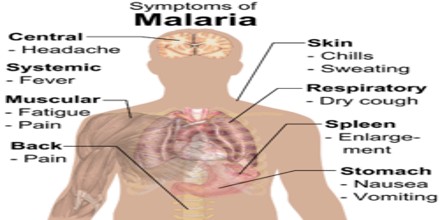
Malaria is an acute febrile illness. In a non-immune individual, symptoms usually appear 10–15 days after the infective mosquito bite. The first symptoms – fever, headache, and chills– may be mild and difficult to recognize as malaria. If not treated within 24 hours, P. falciparum malaria can progress to severe illness, often leading to death.
Children with severe malaria frequently develop one or more of the following symptoms: severe anaemia, respiratory distress in relation to metabolic acidosis, or cerebral malaria. In adults, multi-organ involvement is also frequent. In malaria endemic areas, people may develop partial immunity, allowing asymptomatic infections to occur.
Malaria is caused by a type of microscopic parasite that’s transmitted most commonly by mosquito bites.
- Uninfected mosquito. A mosquito becomes infected by feeding on a person who has malaria.
- Transmission of parasite. If you’re the next person this mosquito bites, it can transmit malaria parasites to you.
- In the liver. The parasites then travel to your liver — where some types can lie dormant for as long as a year.
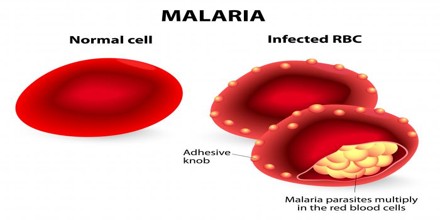
- Into the bloodstream. When the parasites mature, they leave the liver and infect your red blood cells. This is when people typically develop malaria symptoms.
- On to the next person. If an uninfected mosquito bites you at this point in the cycle, it will become infected with your malaria parasites and can spread them to the next person it bites.

Diagnosis, Treatment and Prevention
Early diagnosis of malaria is critical for a patient’s recovery. Any individual showing signs of malaria should be tested immediately. The WHO strongly advises parasitological confirmation by microscopy or a rapid diagnostic test (RDT). The signs and symptoms of the disease are non-specific. However, malaria is clinically suspected on the basis of fever, or a history of fever. Unfortunately, there is no combination of symptoms that can reliably distinguish the disease from other causes, hence the importance of a parasitological test.
The best available treatment, particularly for Plasmodium. Falciparum malaria is artemisinin-based combination therapy (ACT). Simple or uncomplicated malaria may be treated with oral medications. Expanding the access to ACTs has been integral to the global fight against the disease. In 2013, 392 million ACT treatment courses were obtained by endemic countries, a substantial rise from 11 million in 2005. There is growing concern about the increase of cases of malaria resistant to the effects of ACTs. As of February 2015, artemisinin resistance has been confirmed in five countries: Cambodia, Laos, Myanmar, Thailand and Vietnam. For these cases, individuals were still successfully treated, but the ACT must contain an effective partner drug. The WHO has warned that as no alternatives to artemisinin are likely to become available for several years, and because ACTs are the main treatment for P. falciparum malaria, it is of paramount importance that steps be taken to prevent the spread of ACT-resistant strains.

Vector control is the main way to prevent and reduce malaria transmission. If coverage of vector control interventions within a specific area is high enough, then a measure of protection will be conferred across the community.
WHO recommends protection for all people at risk of malaria with effective malaria vector control. Two forms of vector control – insecticide-treated mosquito nets and indoor residual spraying – are effective in a wide range of circumstances.