Hepatopulmonary Syndrome (HPS)
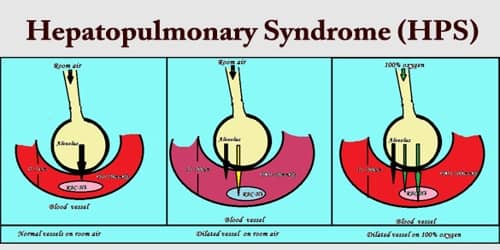
Definition: Hepatopulmonary Syndrome (HPS) is a syndrome of shortness of breath and hypoxemia caused by pulmonary microvascular vasodilation in patients with portal hypertension; dyspnea and hypoxemia are worse when the patient is upright. The problem is that when the liver is not working properly, the blood vessels in the lungs, called capillaries, become enlarged, or “dilated.”
Hepatopulmonary syndrome is caused by blood vessels in the lungs expanding (dilating) and increasing in number, making it hard for red blood cells to properly absorb oxygen. This leaves the lungs unable to deliver adequate amounts of oxygen to the body, which leads to low oxygen levels (hypoxemia).
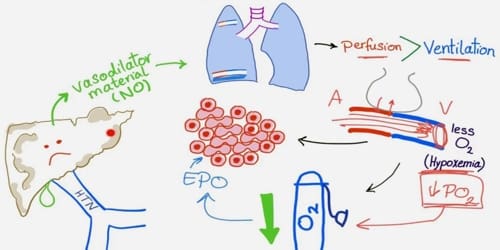
Hepatopulmonary syndrome (HPS) results from the formation of microscopic intrapulmonary arteriovenous dilations in patients with chronic liver disease. The mechanism is unknown but is thought to be due to increased hepatic production or decreased hepatic clearance of vasodilators. The vascular dilations cause overperfusion relative to ventilation, leading to hypoxemia, particularly because patients have an increased cardiac output resulting from systemic vasodilation.
In a healthy person, red blood cells pass through the small blood vessels in the lungs, picking up oxygen from the air inside the lungs. This oxygen is then able to travel to supply the rest of the body. In hepatopulmonary syndrome, the small blood vessels in the lungs become dilated or wider and the oxygen is no longer able to reach all the red blood cells within the vessel. This means that less oxygen is absorbed from the lungs.
Causes, Signs, and Symptoms of HPS: Hepatopulmonary Syndrome (HPS) can cause low oxygen levels in our blood. Having low oxygen levels in our blood means people with HPS experience shortness of breath, which can become more and more severe over time.
The hepatopulmonary syndrome (HPS) results from the formation of microscopic intrapulmonary arteriovenous dilatations in patients with both chronic and far less common, acute liver failure. The mechanism is unknown but is thought to be due to increased liver production or decreased the liver clearance of vasodilators, possibly involving nitric oxide.
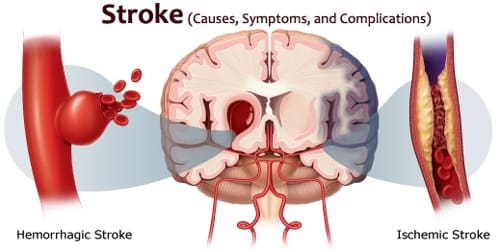
While many people with HPS don’t have any obvious problems, the main reported symptom is shortness of breath (dyspnea) that is worse when standing or sitting up and is relieved when lying down (platypnea). Symptoms related to chronic liver disease (generally cirrhosis) include small red spots on the skin (spider angiomas) and abnormal vascular dilatations. Some other symptoms that have been described are infections in the brain (brain abscesses), brain bleeding and an increased number of red blood cells in the blood (polycythemia).

Diagnosis and Treatment of HPS: Hepatopulmonary syndrome (HPS) consists of the triad of liver dysfunction, otherwise unexplained hypoxemia, and intrapulmonary vascular dilation (IPVD).
A useful diagnostic test is contrasted echocardiography. Intravenous microbubbles from agitated saline that are normally trapped in the pulmonary capillaries rapidly (ie, within 7 heartbeats) traverse the lung and appear in the left atrium. Similarly, IV technetium-99m–labeled albumin may traverse the lungs and appear in the kidneys and brain. Pulmonary angiography may reveal a diffusely fine or blotchy vascular configuration. Angiography is generally not needed unless thromboembolism is suspected.
There is currently no effective medication for HPS. Oxygen therapy may improve breathing in some cases. Other therapies, such as somatostatin to inhibit vasodilation, are of modest benefit in only some patients. Coil embolization is virtually impossible because of the number and size of the lesions. Inhaled nitric oxide synthesis inhibitors may be a future treatment option. Hepatopulmonary syndrome may regress after liver transplantation or if the underlying liver disease subsides.
Prognosis is poor without treatment (survival < 2 yr). The prognosis in hepatopulmonary syndrome is mainly determined by whether or not a liver transplant can be performed. The majority of patients with the hepatopulmonary syndrome have gradually worsening shortness of breath and oxygen levels over time until they get a liver transplant. With liver transplantation, the 5-year survival rate is 74%, which is comparable to patients who undergo liver transplants who do not suffer from the hepatopulmonary syndrome.
Information Source: