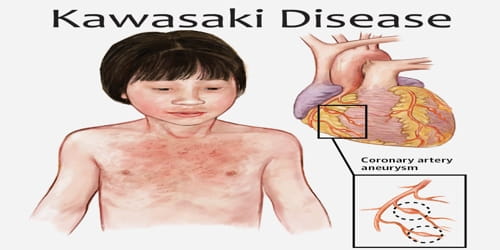
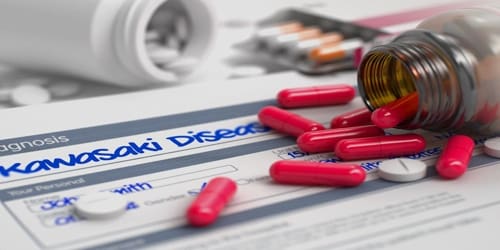
Kawasaki Disease
Definition: Kawasaki disease (KD) or mucocutaneous lymph node syndrome is a rare childhood disease. It is an illness that causes inflammation in arteries, veins, and capillaries. It almost always affects kids, most of them under the age of 5. It’s one of the leading causes of heart disease in children.
The most common symptoms include a fever that lasts for more than five days not affected by usual medications, large lymph nodes in the neck, a rash in the genital area, and red eyes, lips, palms or soles of the feet. Other symptoms include a sore throat and diarrhea. Within three weeks of the onset of symptoms, the skin from the hands and feet may peel. Recovery then typically occurs. In some children, coronary artery aneurysms may form in the heart after 1–2 years.
The Kawasaki Disease Foundation (KDF) estimates that KD affects more than 4,200 children in the United States each year. KD is also more common in boys than in girls and in children of Asian and Pacific Island descent. However, KD can affect children and teenagers of all racial and ethnic backgrounds.
Kawasaki disease is rare. It affects between 8 and 67 per 100,000 people under the age of five except in Japan where it affects 124 per 100,000. It is much less common after the age of five. Boys are more commonly affected than girls. The disorder was first described in 1967 by Tomisaku Kawasaki in Japan.
Causes, Sign, and Symptoms of Kawasaki Disease: As the cause(s) of Kawasaki disease remains unknown, the illness is more accurately referred to as Kawasaki syndrome. Its cause is widely hypothesized to involve the interaction of genetic and environmental factors, possibly including an infection in combination with the genetic predisposition to an autoimmune mechanism. When a child has Kawasaki disease, the blood vessels throughout his body become inflamed. This can damage the coronary arteries, the vessels that carry blood to his heart.

But Kawasaki disease doesn’t affect just the heart. It can also cause problems with lymph nodes, skin, and lining of the mouth, nose, and throat.
Kawasaki disease often begins with a high and persistent fever that is not very responsive to normal treatment with paracetamol (acetaminophen) or ibuprofen. It is the most prominent symptom in Kawasaki disease, is a characteristic sign of the acute phase of the disease, is normally high (above 39–40 °C), is remittent, and is followed by extreme irritability.
Early symptoms, which can last up to two weeks, may include:
- high fever that persists for five or more days
- rash on the torso and groin
- bloodshot eyes, without crusting
- bright red, swollen lips
- “strawberry” tongue, which appears shiny and bright with red spots
- swollen lymph nodes
- swollen hands and feet
- red palms and soles of the feet
Scientists haven’t found an exact cause for Kawasaki disease. But they think it’s probably linked to a combination of genetics, exposure to viruses and bacteria, and other environmental factors, such as chemicals and irritants.
If any child has a fever between 101 and 103 degrees that lasts more than 4 days and shows several of the symptoms noted, contact his doctor. Treating him early can help reduce his chances of any permanent effects.
Diagnosis and Treatment of Kawasaki Disease: Kawasaki disease can’t be passed from one child to another. There is no single test. To diagnose it, doctors look at the signs and symptoms. They may also use an echocardiogram or other tests. It is mainly treated with medicines. Rarely, medical procedures and surgery also may be used for children whose coronary arteries are affected.
A pediatrician might order additional tests to check how the disease has affected the heart. These may include:
- Echocardiograph: An echocardiography is a painless procedure that uses sound waves to create pictures of the heart and its arteries. This test may need to be repeated to show how Kawasaki disease has affected the heart over time.
- Blood tests: Blood tests may be ordered to rule out other illnesses. In KD, there may be an elevated white blood cell count, low red blood cell count, and inflammation.
- Chest X-ray: A chest X-ray creates black and white images of the heart and lungs. A doctor may order this test to look for signs of heart failure and inflammation.
- Electrocardiogram: An electrocardiogram, or ECG, records the electrical activity of the heart. Irregularities in the ECG may indicate that the heart has been affected by KD.
Many children, especially infants, eventually diagnosed with Kawasaki disease, do not exhibit all of the above criteria. The diagnosis can be made purely by the detection of coronary artery aneurysms in the proper clinical setting.
Children with Kawasaki disease should be hospitalized and cared for by a physician who has experience with this disease. Salicylate therapy, particularly aspirin, remains an important part of the treatment (though questioned by some) but salicylates alone are not as effective as IVIG. Aspirin therapy is started at high doses until the fever subsides, and then is continued at a low dose when the patient returns home, usually for two months to prevent blood clots from forming. In cases of Kawasaki disease refractory to IVIG, cyclophosphamide and plasma exchange have been investigated as possible treatments, with variable outcomes.
Timing is critical for preventing serious heart problems. Studies also report a higher rate of resistance to treatment when it’s given before the fifth day of the fever. About 11 to 23 percent of children with KD will have a resistance.
Some children may require longer treatment time to prevent a blocked artery or a heart attack. In these cases, treatment involves daily antiplatelet aspirin doses until they have a normal echocardiograph. It may take six to eight weeks for coronary artery abnormalities to reverse.
Information Source: