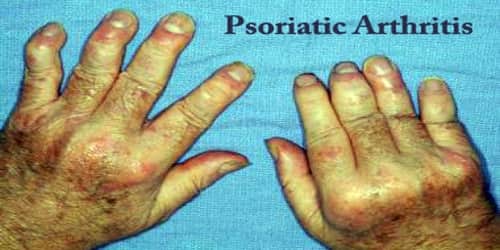
Psoriatic Arthritis
Definition: Psoriatic arthritis (PsA) is a chronic autoimmune disease characterized by a form of inflammation of the skin (psoriasis) and joints (inflammatory arthritis). The classic feature of psoriatic arthritis is swelling of entire fingers and toes with a sausage-like appearance.
Signs and symptoms include patchy, raised, red areas of skin inflammation with scaling. Psoriasis often affects the tips of the elbows and knees, the scalp and ears, the navel, and around the genital areas or anus.
The disease may lay dormant in the body until triggered by some outside influence, such as a common throat infection. Another theory suggesting that bacteria on the skin triggers the immune response that leads to joint inflammation has yet to be proven.
Psoriatic arthritis affects up to 30% of people with psoriasis and occurs in both children and adults. Approximately 40–50% of individuals with psoriatic arthritis have the HLA-B27 genotype. The condition is less common in people of Asian or African descent and affects men and women equally.
No cure for psoriatic arthritis exists, so the focus is on controlling symptoms and preventing damage to patient’s joints. Without treatment, psoriatic arthritis may be disabling.
Types of Psoriatic Arthritis: The type of psoriatic arthritis depends on the distribution of the joints affected.
There are five types of psoriatic arthritis:
- Symmetric PsA: This makes up about 50 percent of psoriatic arthritis cases. Symmetric means it affects joints on both sides of the body at the same time. This type of arthritis is similar to rheumatoid arthritis (RA).
- Asymmetric PsA: Often mild, this type of PsA appears in 35 percent of people with the condition. It’s called asymmetric because it doesn’t appear in the same joints on both sides of the body.
- Distal interphalangeal predominant PsA: This type causes inflammation and stiffness near the ends of the fingers and toes, along with changes in toenails and fingernails such as pitting, white spots and lifting from the nail bed.
- Spondylitis PsA: This type of PsA involves the patient’s spine. Patient’s entire spine from their neck to their lower back may be affected. This can make movement very painful. Patient’s hands, feet, legs, arms, and hips may also be affected.
- Psoriatic arthritis mutilans: This is a severe, deforming type of PsA. About 5 percent of people with PsA have this type. Psoriatic arthritis mutilans usually affects the patient’s hands and feet. It can also cause pain in your neck and lower back.

Causes, Sign, and Symptom of Psoriatic Arthritis: Psoriatic arthritis (PsA) occurs when our body’s immune system begins to attack healthy cells and tissue. The abnormal immune response causes inflammation in our joints as well as overproduction of skin cells.
PsA runs in families. About 40 percent of people with the condition have one or more relatives with PsA. Something in the environment usually triggers the disease for those with a tendency to develop PsA. That could be a virus, extreme stress, or an injury.
In patients with psoriatic arthritis who have arthritis of the spine, a blood test gene marker called HLA-B27 is found in about 50%. Several other genes have also been found to be more common in patients with psoriatic arthritis. The signs and symptoms of psoriatic arthritis often resemble those of rheumatoid arthritis. Both diseases cause joints to become painful, swollen and warm to the touch.
Symptoms of PsA are different for each person. They can be mild to severe.
General symptoms of PsA include:
- swollen, tender joints on one or both sides of our body
- morning stiffness
- swollen fingers and toes
- painful muscles and tendons
- scaly skin patches, which may get worse when joint pain flares up
- flaky scalp
- fatigue
- nail pitting
- separation of our nail from the nail bed
- eye redness (conjunctivitis)
- eye pain (uveitis)
Psoriatic arthritis may remain mild or may progress to more destructive joint disease. Periods of active disease, or flares, will typically alternate with periods of remission. In severe forms, psoriatic arthritis may progress to arthritis mutilans which on X-ray gives a “pencil-in-cup” appearance.

Diagnosis and Treatment of Psoriatic Arthritis: There is no definitive test to diagnose psoriatic arthritis. Symptoms of psoriatic arthritis may closely resemble other diseases, including rheumatoid arthritis. A rheumatologist (a doctor specializing in autoimmune diseases) may use physical examinations, health history, blood tests, and x-rays to accurately diagnose psoriatic arthritis.
No cure exists for psoriatic arthritis, so treatment focuses on controlling inflammation in patients affected joints to prevent joint pain and disability.
Generally, the treatment of arthritis in psoriatic arthritis involves a combination of anti-inflammatory medications (NSAIDs) and exercise. Exercise programs can be done at home or with a physical therapist and are customized according to the disease and physical capabilities of each patient.
Non-steroidal anti-inflammatory drugs (NSAIDs) are a group of medications that are helpful in reducing joint inflammation, pain, and stiffness. Examples of NSAIDs include aspirin, indomethacin (Indocin), tolmetin sodium (Tolectin), sulindac (Clinoril), and diclofenac (Voltaren). Their most frequent side effects include stomach upset and ulceration. The drugs can also cause gastrointestinal bleeding.
Retinoid etretinate is effective for both arthritis and skin lesions. Photochemotherapy with methoxy psoralen and long-wave ultraviolet light (PUVA) are used for severe skin lesions. Doctors may use joint injections with corticosteroids in cases where one joint is severely affected.
Information Source: